When living with chronic kidney disease (CKD), creating a care plan that includes a well-balanced diet is essential to maintaining kidney health and preventing further damage. Healthy eating plays a critical role in managing CKD, as it helps control key factors like blood pressure, blood sugar, and nutrient levels that can impact kidney function. Here’s a comprehensive guide to eating healthy for chronic kidney disease: Here is more information on CKD for Older Adults , and here is more on Trending Topics on Kidney Disease.

1. Low Protein for Kidney Protection
- Reducing protein intake can help lessen the burden on your kidneys. While protein is essential for overall health, consuming excessive amounts can lead to further kidney damage.
- Your diet for chronic kidney disease should focus on moderate protein sources like eggs, fish, or lean poultry in controlled portions, tailored to your stage of CKD.
2. Monitor Sodium Intake
2.1 Impact of Excessive Sodium:
- Fluid Retention: High sodium intake causes the body to retain more water, which can lead to swelling (edema) in the legs, ankles, and face.
- High Blood Pressure: Excess sodium can raise blood pressure, which is a common issue for people with kidney disease. Elevated blood pressure further damages the kidneys and accelerates the progression of CKD.
- Increased Workload on Kidneys: When kidneys cannot effectively filter excess sodium, it increases the workload on the kidneys and can lead to kidney function decline over time.
2.2 Recommended Sodium Intake for Kidney Disease:
- For individuals with chronic kidney disease (CKD), the recommended sodium intake is generally less than 2,300 milligrams (mg) per day, and in some cases, even lower (around 1,500 mg per day) if blood pressure or fluid retention is a concern.
2.3. Moderation, Not Elimination:
- While reducing salt can help lower blood pressure, going to extremes—such as a dangerously low sodium intake—may lead to other health issues like hyponatremia or poor appetite.
- Practical Tip: Gradually reduce (not eliminate) salt and flavor foods with herbs, spices, lemon juice, or vinegars for taste.
3. Control Potassium Levels
Potassium management is essential for CKD patients, as too much or too little can cause complications.
- High-Potassium Foods to Avoid: Bananas, oranges, brown rice, beans, and nuts.
- Low-Potassium Alternatives to Include: Apples, peaches, green beans, white bread, and grapes.
Your healthcare provider can guide you on the appropriate potassium intake for your specific condition.
4. Limit Fats and Alcohol
4.1. Do’s and Don’ts for Managing CKD
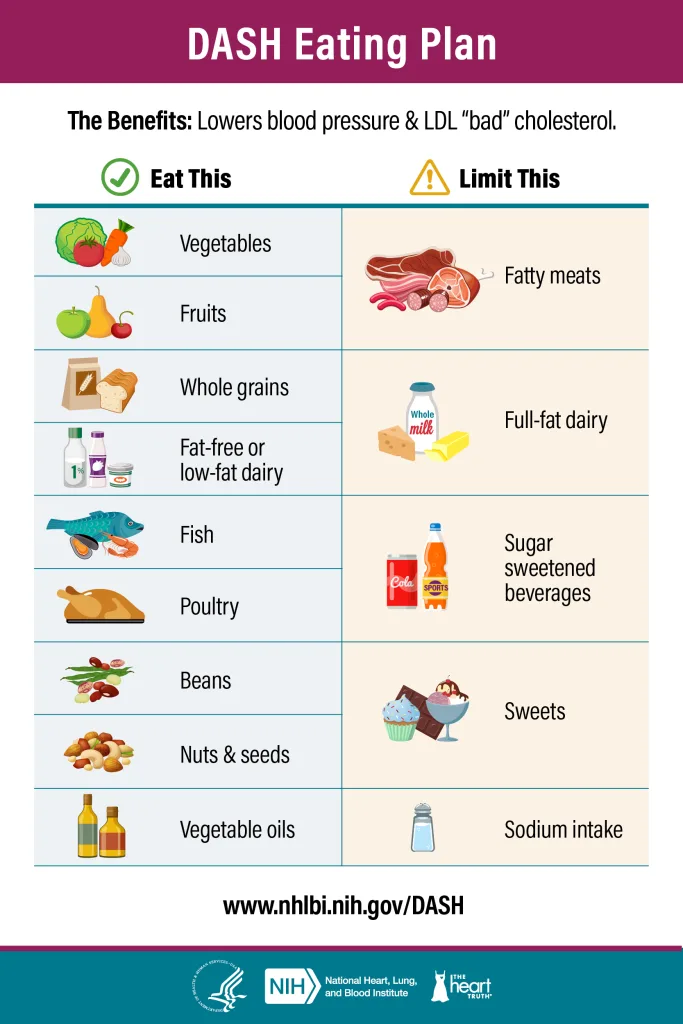
Do’s >> Eat This
- DO choose healthy fats: Include unsaturated fats from sources like olive oil, avocado, nuts (in moderation), and seeds.
- DO limit saturated fats: Opt for low-fat or non-fat dairy products, lean meats, or plant-based alternatives.
- DO use healthy cooking methods: Bake, grill, or steam foods instead of frying.
- DO include omega-3 fatty acids: Incorporate fish like salmon or plant-based sources like flaxseeds and walnuts.
- DO read food labels: Check for trans fats and avoid products with hydrogenated oils. Follow DASH diet since avoiding high blood pressure and bad cholesterol is crucial for managing CKD >>
Don’ts >> Limit This
- DON’T consume trans fats: Steer clear of fried foods, margarine, and processed snacks like chips or cookies.
- DON’T overeat high-fat animal products: Reduce intake of fatty cuts of meat, full-fat dairy, and butter.
- DON’T overeat healthy fats: Even healthy fats are calorie-dense, so consume them in moderation.
- DON’T rely on overly processed foods: Minimize consumption of fast foods and ready-to-eat meals high in unhealthy fats.
- DON’T ignore cholesterol levels: Monitor and avoid foods high in dietary cholesterol if advised by your doctor.
4.1 Unsaturated Fats
What are unsaturated fats?
- Unsaturated fats are healthy fats that stay liquid at room temperature
- Commonly found in foods like olive oil, avocados, nuts, seeds, and fatty fish like salmon.
- They can help lower bad cholesterol (LDL) and support heart health when eaten in place of saturated fats.
- Sources: Olive oil, avocados, nuts, seeds, fatty fish (e.g., salmon, mackerel, tuna).
- Benefits:
- Heart Health: CKD patients are at higher risk of cardiovascular disease, and unsaturated fats help lower LDL (“bad”) cholesterol while raising HDL (“good”) cholesterol.
- Anti-Inflammatory: Omega-3 fatty acids, a type of unsaturated fat, reduce inflammation, which can help slow CKD progression and reduce the risk of heart disease.
- Weight Management: These fats are nutrient-dense, helping to maintain energy levels without adding unnecessary weight, which can strain kidney function.
4.2 Limit Saturated Fats
What are Saturated Fats?
- Saturated fats are usually found in animal products (e.g., butter, cheese, fatty meats) and some plant oils (e.g., coconut and palm oil).
- You can tell if something is a saturated fat if it is solid at room temperature.
- Overconsumption can raise LDL “bad” cholesterol levels, increasing the risk of heart disease.
- Animal-Based Foods:
- Fatty Meats: Beef, pork, lamb, and processed meats like sausages, bacon, and hot dogs.
- Dairy Products: Whole milk, butter, cream, cheese, and full-fat yogurt.
- Poultry Skin: Chicken and turkey skin are rich in saturated fat.
- Lard and Tallow: Used in traditional cooking and baking.
- Plant-Based Sources:
- Coconut Products: Coconut oil, coconut milk, and cream are high in saturated fats.
- Palm Oil: Commonly used in processed foods like cookies, crackers, and instant noodles.
- Cocoa Butter: Found in chocolate and some baked goods.
- Processed and Fast Foods:
- Fried Foods: Deep-fried snacks, chicken, and french fries.
- Baked Goods: Pastries, cakes, donuts, and cookies often contain saturated fat from butter, cream, or shortening.
- Convenience Foods: Frozen pizzas, prepackaged meals, and snack bars.
Risks of Eating Too Much Saturated Fat in CKD
- Cardiovascular Disease:
- CKD increases the risk of heart disease, and saturated fats contribute to higher LDL (“bad”) cholesterol levels.
- Excess LDL can lead to plaque buildup in arteries (atherosclerosis), heightening the risk of heart attacks or strokes.
- Inflammation:
- High saturated fat intake can promote systemic inflammation, which may exacerbate kidney damage and accelerate CKD progression.
- Weight Gain and Obesity:
- Saturated fats are calorie-dense, and excessive consumption can lead to weight gain.
- Obesity further strains the kidneys, increasing the risk of hypertension and diabetes, which are leading causes of CKD.
- Worsened Lipid Profile:
- CKD patients often have altered lipid metabolism, making it harder to process excess saturated fats.
- This imbalance can contribute to dyslipidemia (abnormal cholesterol levels), a condition common in CKD patients.
- Phosphorus and Potassium Concerns:
- Many foods high in saturated fats, such as full-fat dairy and processed meats, are also high in phosphorus and potassium.
- CKD patients often need to limit these nutrients to prevent complications like hyperphosphatemia or hyperkalemia.
Excessive fats and alcohol can contribute to high blood pressure and diabetes—two leading causes of CKD. Choose healthy fats like those from avocados or olive oil in small amounts, and minimize alcohol consumption to protect your kidney health. Knowing the difference between saturated and unsaturated fats is crucial to staying healthy. Read an article from Harvard Health about how much saturated, trans, and unsaturated fats is healthy.
4.3 Avoid Trans-Fats
- Sources: Processed foods, fried foods, margarine, baked goods made with hydrogenated oils.
- Risks:
- Significantly raise LDL “bad” cholesterol and lower HDL “good” cholesterol, worsening heart disease risk.
- Associated with systemic inflammation, which negatively affects kidney function and overall health.
4.4 Avoid Alcohol
Why Limit Alcohol?
- Kidney Strain: Alcohol increases the kidneys’ workload, worsening damage.
- Dehydration: Alcohol acts as a diuretic, reducing blood flow to the kidneys.
- Blood Pressure: Alcohol raises blood pressure, a leading cause of CKD.
- Medication Interference: Alcohol can reduce the effectiveness of CKD medications.
- Electrolyte Imbalance: It disrupts sodium and potassium levels, which are already hard to manage in CKD.
Guidelines for CKD Patients
- Limit Intake: If approved by a doctor, stick to moderate consumption—no more than 1 drink/day for women, 2 for men.
- Stay Hydrated: Drink water alongside alcohol to prevent dehydration.
- Choose Wisely: Avoid high-sodium mixers and binge drinking.
- Opt Out When Needed: In advanced CKD, liver disease, or with certain medications, avoid alcohol entirely.
5. Stay Hydrated, but Not Overhydrated
Getting the Optimal Amount of Hydration for Kidney Disease
Drink water consistently throughout the day, but avoid excessive amounts in one sitting to reduce strain on the kidneys.
Individualized Fluid Recommendations:
- The optimal amount of fluid depends on the stage of kidney disease, overall health, and individual needs.
- Early CKD: A moderate fluid intake is generally recommended, but it should be adjusted based on urine output and kidney function.
- Advanced CKD: Fluid intake may need to be limited to prevent fluid buildup, often guided by a healthcare provider or dietitian.
Guidelines:
- Aim for about 8 cups (64 ounces) of fluid a day, unless otherwise instructed by a healthcare provider. This may include water, herbal teas, and broths.
- Limit high-sodium beverages (e.g., salty soups, sports drinks) to prevent fluid retention.
6. Essential Vitamins for Chronic Kidney Disease Management
These vitamins are particularly important for CKD patients as the disease can impair the absorption of these nutrients. Monitoring and managing vitamin levels with the help of a healthcare provider is crucial to prevent deficiencies and complications. A kidney-friendly diet and proper supplementation are key to improving quality of life and slowing CKD progression.
- Vitamin D: Crucial for bone health; CKD can impair the kidneys’ ability to convert vitamin D into its active form. Supplementing with active vitamin D (calcitriol) helps regulate calcium and phosphate levels, reducing the risk of bone disease.
- Source: sunlight, cereals, plant-based milks(oat or almond milk)
- Vitamin B12: Important for red blood cell production; helps combat anemia, which is common in CKD patients. CKD patients often have a B12 deficiency because it is often consumed through protein sources like poultry and egg yolks.
- Source: Fortified Nutritional Yeast, fortified cereals, B12 supplements
- Folic Acid: Works with vitamin B12 to support red blood cell health and prevent anemia.
- Source: Cabbage or iceberg lettuce, fortified pasta or bread
- Vitamin C: Boosts immune function but should be managed carefully, as excess intake can increase the risk of kidney stones in people with CKD.
- Source: citrus fruits(oranges), potatoes, tomatoes, red bell pepper, broccoli
- Vitamin E: A powerful antioxidant that reduces inflammation and oxidative stress, which are often elevated in CKD.
- Source: Unsalted nuts or seeds (ex: sunflower seeds), zuchinni, yellow squash, spinnach
7. Personalize Your Care Plan
7.1 On Dialysis

A low-protein diet is recommended for individuals with kidney disease who are not on dialysis to reduce stress on the kidneys and potentially slow the progression of kidney function loss. Including more plant-based foods can also be beneficial. However, for those on dialysis, a higher protein intake is necessary to maintain blood protein levels and overall health, as dialysis removes protein waste from the blood.
If you are on dialysis, being on a high protein diet is necessary to maintain blood protein levels. Learn more about specific protein needs in this fact sheet.
7.2 Vegan or vegetarian diets
Benefits of Vegan/Vegetarian Diets for CKD
- Heart Health: Low in saturated fats, reducing cardiovascular risk.
- Rich in Nutrients: High in fruits, vegetables, and antioxidants that support overall health.
- Improved Blood Pressure: Potassium, fiber, and magnesium can help manage blood pressure.
- Weight Management: Low-calorie foods assist with maintaining a healthy weight.
- Reduced Diabetes Risk: Helps prevent or manage diabetes, which is common in CKD.
Considerations for CKD on Vegan/Vegetarian Diets
- Potassium/Phosphorus: Many plant foods are high in potassium and phosphorus; monitor intake to avoid complications.
- Vitamin B12 Deficiency: Vegan diets lack B12; consider supplements or fortified foods.
- Iron Absorption: Plant-based iron is less absorbed; pair with vitamin C or take supplements.
- Omega-3 Fatty Acids: Plant sources may not provide enough; consider supplements.
- Calcium Intake: Ensure sufficient calcium from fortified foods or supplements.
- Fluid Balance: Monitor fluid intake from both drinks and water-rich foods.
Every individual with CKD is unique, so your diet should be part of a broader care plan tailored to your condition and lifestyle. Consult with a registered dietitian or healthcare provider to ensure your nutritional needs are met while protecting your kidney health.
8. Key Takeaways
- Limit Protein: Reducing protein intake helps reduce kidney strain and prevents the buildup of waste products in the blood. Make sure to get your protein from lean meats like poultry and fish.
- Take Measures to Prevent Secondary Disorders: Monitor and manage conditions like high blood pressure, diabetes, and heart disease, which can worsen kidney function by avoiding processed foods and alcohol. Their high sodium content and trans-fats risk these diseases.
- Manage Fluid Intake: Ensure proper hydration without overloading the kidneys, adjusting based on kidney function and health needs. Avoid soups and salty broths.
- Listen to Your Care Provider or Doctor: Follow personalized guidance from healthcare professionals to manage CKD effectively and prevent complications.
By prioritizing a kidney-friendly diet and making thoughtful choices, you can take an active role in managing chronic kidney disease (CKD) and improving your quality of life. For more information, visit trusted resources like MedlinePlus or the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
By incorporating these dietary guidelines into your daily routine, you can help protect your kidneys and support overall health while living with CKD.
Share your experiences and learn from others in the community >> Join the Conversation On Kidney Disease.