Why Healthy Eating for Osteoarthritis?
Osteoarthritis (OA) or Joint Pain is a common joint disorder among older adults. It involves the gradual breakdown of cartilage that cushions the ends of the bones, leading to pain, stiffness, and reduced mobility. Research consistently shows that dietary choices and healthy eating for osteoarthritis play a significant role in managing arthritis . Here is more information on Osteoarthritis / Joint Pain , and here is more on Trending Topics on Osteoarthritis / Joint Pain.
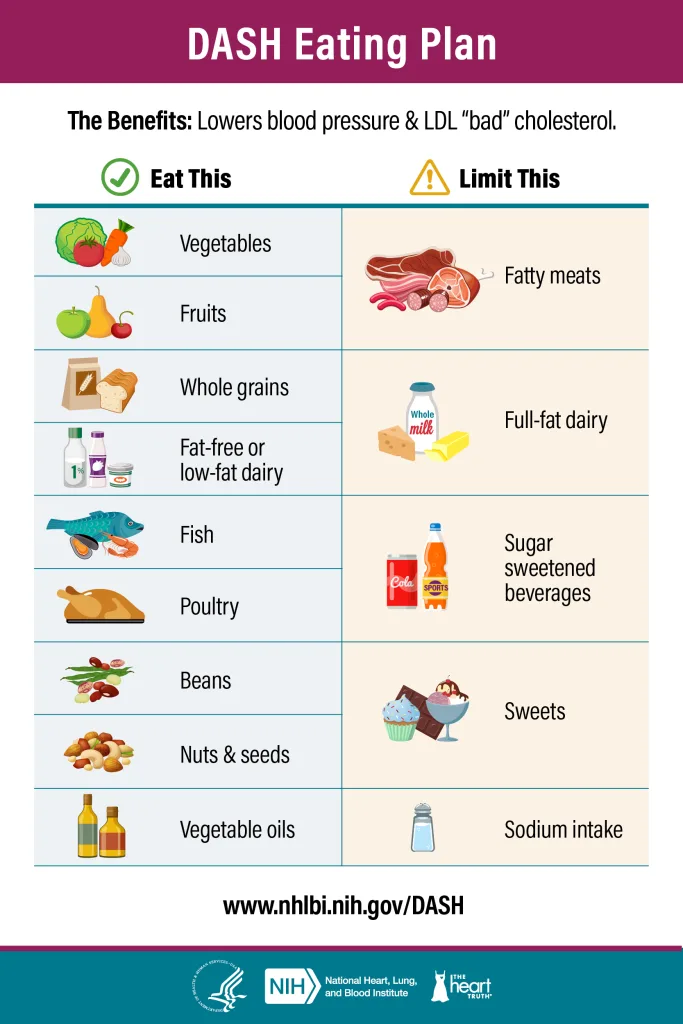
There are two key aspects to healthy eating for osteoarthritis. First, focus on anti-inflammatory foods, such as omega-3-rich fish, and nutrients essential for joint health, like calcium and vitamin D. Second, adopt the DASH diet to support better blood pressure management. This dual approach is beneficial for two reasons:
- Reducing Inflammation: High levels of LDL (“bad”) cholesterol and overall high cholesterol are linked to increased inflammation in the body. Chronic, low-grade inflammation can worsen osteoarthritis symptoms by accelerating cartilage breakdown and increasing joint discomfort.
- Heart-Healthy Equals Joint-Healthy: Dietary changes that improve cholesterol levels—such as incorporating more fruits, vegetables, whole grains, and healthy fats—not only reduce inflammation but also support weight management and balanced nutrient intake. Maintaining a healthy weight reduces stress on weight-bearing joints, like the knees and hips, which can help alleviate osteoarthritis symptoms.hips—aggravating OA symptoms.
2. General Dietary Recommendation
2.1. Do’s and Don’ts for Managing Arthritis
Do’s >> Eat This
- Prioritize Anti-Inflammatory Foods: Include omega-3-rich foods such as fatty fish (salmon, mackerel, sardines), flaxseeds, chia seeds, and walnuts to combat inflammation. Add turmeric and ginger for their natural anti-inflammatory properties.
- Focus on Joint-Supporting Nutrients with Calcium and Vitamin D: Ens fortified plant-based milks, dairy, leafy greens, and eggs.Vitamin C: Include citrus fruits, bell peppers, and strawberries to support cartilage repair.
- Do focus on whole, minimally processed foods, watch your portions to maintain a healthy weight
- Do Extra Virgin Olive Oil
- Anthocyanin-Rich Foods: cherries, blueberries, and blackberries
- Do stay hydrated; water helps maintain kidney function and overall circulation.
- Do consider low-fat dairy if appropriate, as it provides calcium which may help lower blood pressure.
- Follow DASH diet while emphasizing ^^
Don’ts >> Limit This
- Don’t Sugars. Don’t forget about hidden sugars in beverages, sauces, and snacks.
- Don’t Red Meats & Processed Meats. arthritis-friendly diets go a step further than DASH to limit red and processed meats due to their potential inflammatory effects
- Don’t intake of omega-6-rich oils (e.g., corn oil, sunflower oil) as an imbalance between omega-6 and omega-3 fats promote inflammation.
- Don’t nightshades (tomatoes, potatoes, eggplants, and peppers). While evidence is anecdotal, pay attention to whether these trigger symptoms for you.
- Avoid Extreme Calorie Deficits: arthritis management warns against overly restrictive diets that could result in nutrient deficiencies (e.g., calcium, vitamin D) critical for joint health
- Don’t Saturated Fats like Butter. Don’t overheat oil
- Don’t overdo alcohol; moderate intake is key.
- Don’t ignore advice from your healthcare provider about medication and diet—both are crucial.
2.2. Which Oils to Use for Better Osteoarthritis Maintenance
For better osteoarthritis maintenance and Healthy Eating for Osteoarthritis, the oils you use should primarily support anti-inflammatory properties and promote joint health. Here’s a breakdown of the best oils and their benefits:
- Extra Virgin Olive Oil
- Studies show that olive oil reduces markers of inflammation and benefits joint health.
- Olive Oil is rich in oleocanthal, a compound with anti-inflammatory properties similar to ibuprofen. High in monounsaturated fats, which help reduce inflammation and support heart health.
- Usage: Use for cooking at low to medium heat, drizzling over salads, or as a base for dressings.
- Avocado Oil
- High in monounsaturated fats and antioxidants. Contains compounds that may support cartilage repair.
- Usage: Stable at high heat, making it versatile for cooking. Ideal for sautéing, baking, or frying due to its high smoke point.
- Flaxseed Oil (Cold-Pressed)
- Excellent source of alpha-linolenic acid (ALA), a plant-based omega-3 fatty acid that can help reduce inflammation. Promotes heart and joint health.
- Usage: Use in dressings, smoothies, or drizzled over foods; not suitable for cooking due to its low smoke point.
- Walnut Oil
- High in omega-3 fatty acids, which may help lower inflammation.
- Usage: Best used in salad dressings or as a finishing oil. Avoid heating it to preserve its nutrients.
- Canola Oil (Cold-Pressed or Non-GMO Preferred)
- Contains a good balance of omega-3 and omega-6 fatty acids, making it a more affordable anti-inflammatory option.
- Usage: Use for baking, sautéing, or as a neutral oil in recipes.
2.3 Oils to Avoid or Limit
- Corn Oil, Soybean Oil, and Sunflower Oil
- High in omega-6 fatty acids, which in excess can promote inflammation.
- Balance is key: Too much omega-6 relative to omega-3 can worsen inflammation.
- Partially Hydrogenated Oils/Trans Fats
- Found in margarine, shortening, and some processed foods.
- Can significantly increase inflammation and are harmful to both joint and heart health.
- Palm Oil
- While not inherently harmful, it lacks the anti-inflammatory properties found in oils like olive or avocado oil.
Choosing the right oils for cooking and eating can make a big difference in managing blood pressure. This guide will help you understand which oils are better for heart health and when to use them.
If You Have Kidney Problems (CKD)
- Be cautious with omega-3-rich oils and limit potassium-rich foods if advised by your doctor. Consult a dietitian for personalized advice.
If You Have Diabetes
Focus on oils that are low in saturated fats and help improve blood sugar levels, like olive oil or canola oil. Avoid oils in processed snacks or fast food, which may worsen insulin resistance.
Emphasize Whole Foods
- Fruits and Vegetables: Aim for a variety of colors—dark leafy greens, berries, citrus fruits, etc. These are rich in potassium, magnesium, and fiber which can help regulate blood pressure.
- Whole Grains: Brown rice, whole-wheat bread, oatmeal, and quinoa provide fiber and essential nutrients.
- Lean Proteins: Skinless poultry, fish, beans, lentils, and legumes offer protein without excessive saturated fats.
2.3. Vitamins and Their Role in Managing High Blood Pressure
Vitamins play a critical role in managing osteoarthritis by supporting joint health, reducing inflammation, and aiding in cartilage repair. Vitamin D is essential for maintaining bone density and joint health, as it helps the body absorb calcium and supports the immune system. Deficiencies in vitamin D are linked to increased joint pain and stiffness. Vitamin C is vital for collagen synthesis, a key component of cartilage, and acts as an antioxidant to reduce oxidative stress and inflammation in the joints. Similarly, Vitamin E, another powerful antioxidant, helps combat free radicals that can worsen joint damage and inflammation. Vitamin K supports bone and cartilage health by aiding in bone mineralization and reducing inflammation markers. While these vitamins can be obtained through a balanced diet, including foods like leafy greens, citrus fruits, nuts, and fortified products, supplementation may be necessary for those with deficiencies. Always consult a healthcare provider before starting supplements to ensure safe and effective use for osteoarthritis management.
3. Maintain healthy body weight, and help reduce excess inflammation. Below are evidence-based strategies:
- Emphasize Whole Foods
- Focus on fruits, vegetables, whole grains, and lean proteins.
- For example, apples, berries, spinach, broccoli, brown rice, quinoa, beans, and chicken breast.
- Resource: Harvard T.H. Chan School of Public Health: The Nutrition Source
- Choose Anti-Inflammatory Fats
- Incorporate sources of Omega-3 fatty acids (e.g., salmon, mackerel, sardines, flaxseeds, walnuts) to help ease inflammation.
- Limit saturated and trans fats (e.g., fried foods, processed snack items).
- Resource: Arthritis Foundation: Best Food for Arthritis
- Optimize Calcium and Vitamin D
- Support bone health through dairy (or fortified dairy alternatives), leafy greens, and safe sun exposure for vitamin D.
- Consider discussing supplements with your healthcare provider if dietary intake is insufficient.
- Resource: NIH Office of Dietary Supplements: Calcium
- Resource: NIH Office of Dietary Supplements: Vitamin D
- Watch Portion Sizes & Maintain a Healthy Weight
- Excess weight places more stress on weight-bearing joints, worsening OA symptoms.
- Use smaller plates, be mindful of portion sizes, and increase daily movement if possible.
- Resource: CDC on Weight Management
- Stay Hydrated
- Dehydration can make joint symptoms feel worse. Aim for at least 6–8 cups of water daily (unless otherwise directed by your physician).
- Resource: Academy of Nutrition and Dietetics: Hydration
A Note on Avoiding Extremes
Some diets dramatically reduce certain nutrients or entire food groups. However, going too far—like cutting out all carbohydrates or fats—can lead to nutrient deficiencies and may worsen symptoms over time. Aim for moderation and a balanced approach.
3. Dietary Considerations for Different Lifestyles
3.1 Vegetarian
- Protein Sources
- Emphasize beans, lentils, chickpeas, tofu, tempeh, eggs (if lacto-ovo), and low-fat dairy (if lacto).
- Calcium & Iron
- Obtain from dark leafy greens, fortified cereals, and milk alternatives (almond, soy, or oat milk).
- Vitamin B12
- May need supplementation if you avoid all animal products except dairy/eggs.
- Resource: Vegetarian Nutrition from the Academy of Nutrition and Dietetics
3.2 Vegan
- Complete Proteins
- Combine different plant proteins (e.g., beans + rice or hummus + whole grain pita) to ensure adequate amino acid intake.
- Omega-3 Fats
- Aim for flaxseeds, chia seeds, walnuts, and algae-based supplements.
- Calcium, Vitamin D, B12
- Pay extra attention to calcium and vitamin D through fortified products. Vitamin B12 supplementation is often necessary.
- Resource: Vegan Society
3.3 Kosher
- Lean Kosher Proteins
- Skinless poultry, fish with fins and scales, lean cuts of kosher beef in moderation.
- Plant-Based Options
- Legumes (beans, peas, lentils) are an important protein source; combine them with whole grains.
- Avoiding Processed Foods
- Many kosher-certified processed foods can be high in sodium. Check labels, especially if you also have high blood pressure.
- Resource: Orthodox Union Kosher
4. Specific Health Conditions
4.1 Osteoarthritis & High Blood Pressure (Hypertension)
- Limit Sodium
- Choose reduced-sodium or “no-salt-added” products. Flavor foods with herbs and spices instead of salt.
- Potassium-Rich Foods
- Bananas, potatoes, avocados, spinach, and other greens can help balance blood pressure.
- Healthy Fats & Whole Grains
- Consider the DASH diet principles, which emphasizes fruits, vegetables, and low-fat dairy. This approach can also benefit OA by maintaining healthy weight.
- Resource:
4.2 Osteoarthritis & Diabetes
- Control Carbohydrate Intake
- Opt for complex carbs (whole grains, legumes) and avoid sugary drinks and processed snacks.
- Moderate Fat Intake
- Focus on healthy fats from nuts, seeds, avocados, and fish.
- Steady, Balanced Meals
- Eat at regular intervals to maintain stable blood sugar levels.
- Resource:
5. Closing Thoughts
Healthy eating for osteoarthritis involves a balanced and flexible approach. Whether you follow a vegetarian, vegan, kosher, or any other diet, focus on whole, minimally processed foods and keep in mind your other health conditions such as high blood pressure or diabetes. Remember that moderation, not extremism, is key: cutting out entire food groups or severely restricting calories can do more harm than good in the long run.
For a personalized plan, always consult with a registered dietitian or your healthcare provider—especially if you have multiple health concerns. Small, consistent changes in your eating habits can significantly impact not only your joint health but also your overall well-being.
Share your experiences and learn from others in the community >> Join the Conversation On Arthritis