Chronic Kidney Disease (CKD) can be a challenging condition, especially for older adults, but you are not alone. Many people face this condition, and support is available to help you manage it. While CKD currently has no cure, managing it effectively is crucial to maintaining your health, preventing complications, and improving your quality of life. Together, with the right care and lifestyle changes, you can navigate this journey. Click here for >> Healthy Eating for Chronic Kidney Disease.
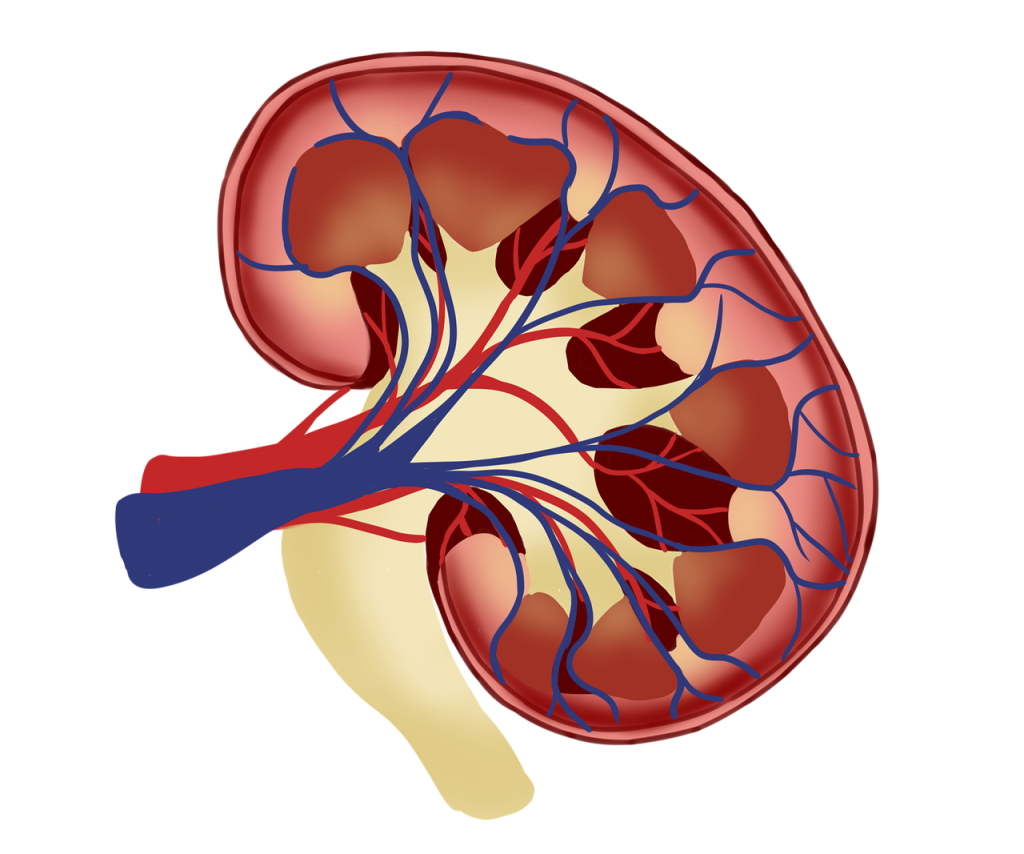
Understanding Chronic Kidney Disease
CKD is a condition where the kidneys lose their ability to filter waste and excess fluids from the blood effectively. This can lead to a buildup of harmful substances in the body. CKD often develops gradually over time and is more common in older adults due to factors like age-related decline in kidney function, diabetes, and high blood pressure.
The symptoms can include:
- Fatigue
- Swelling in the legs or feet
- Frequent urination
- Loss of appetite
- Difficulty concentrating
It’s important to remember that CKD is a progressive condition. Early detection and management can slow its progression and reduce the risk of severe complications.
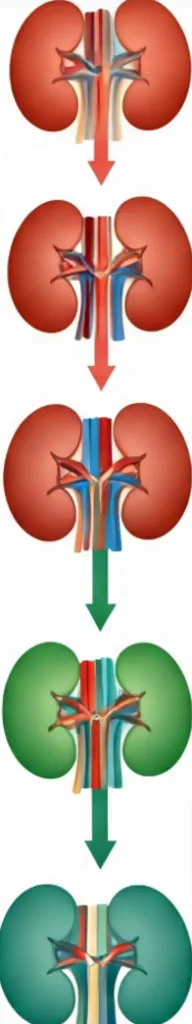
Stages of Chronic Kidney Disease
Chronic Kidney Disease (CKD) is classified into five stages based on the level of kidney function, as indicated by the glomerular filtration rate (how well the kidney can filter the blood, GFR). Here’s an overview of the description and severity for each stage:
What You Can Do to Manage CKD
1. Follow Your Doctor’s Advice
Start by taking any medications prescribed by your doctor exactly as directed. These may include medications to control blood pressure, blood sugar, or manage symptoms like swelling. Regular check-ups are essential to monitor your condition.
2. Adopt a Kidney-Friendly Diet
- Limit salt intake to control blood pressure.
- Avoid high-potassium foods like bananas and oranges if recommended by your doctor.
- Opt for lean proteins such as chicken or fish, but in moderation.
- Stay hydrated, but follow your doctor’s guidance on fluid intake.
- Find more information about a CKD friendly diet at Healthy Eating for Chronic Kidney Disease
3. Incorporate Gentle Exercise
Engage in light activities such as walking or yoga to improve overall health and reduce stress on your kidneys. Always consult your healthcare provider before starting a new exercise routine.
4. Monitor Blood Pressure and Blood Sugar
If you have diabetes or high blood pressure, keep them under control as they are leading causes of CKD.
5. Avoid Over-the-Counter Painkillers
Certain medications like NSAIDs (e.g., ibuprofen) can worsen kidney function. Always check with your doctor before taking any new medication.
Medical Management
Your healthcare provider plays a key role in managing CKD. They may recommend:
- Regular Monitoring: Blood and urine tests to track kidney function.
- Medications: Drugs to control blood pressure, reduce protein loss in urine, or treat anemia.
- Dialysis: In advanced cases, dialysis may be necessary to filter waste from your blood.
While these treatments can have side effects like fatigue or low blood pressure, the risks of untreated CKD—including heart disease and kidney failure—are far greater. Open communication with your healthcare team can help you make informed decisions about your care.
Treatment Challenges
Managing CKD in older adults can come with challenges:
- Polypharmacy: Many older adults take multiple medications, increasing the risk of interactions and side effects.
- Limited Mobility: Traveling for frequent doctor visits or dialysis can be difficult.
- Emotional Impact: The stress of living with a chronic condition can lead to feelings of frustration or depression.
Despite these challenges, advancements in care and supportive resources can make a significant difference.
New Trends and Innovations
Recent advancements offer hope for improved CKD management:
- Artificial Intelligence (AI): AI-driven tools help doctors analyze kidney function and predict disease progression more accurately.
- Wearable Devices: Continuous monitoring devices track vital signs and alert users to potential issues.
- Precision Medicine: Personalized treatment plans based on genetic and lifestyle factors are becoming more common.
- Regenerative Therapies: Research into stem cell treatments and bioengineered kidneys holds promise for the future.
Discover latest trends and innovation in more detail here: New Trends in Chronic Kidney Disease For Older Adults
Financial Guidance
Managing CKD can be expensive, but there are resources available:
- Medicare and Medicaid: These programs often cover CKD-related treatments.
- Nonprofit Organizations: Groups like the National Kidney Foundation provide financial assistance and support.
- Discount Programs: Ask your doctor or pharmacist about generic medications and discount cards.
- Community Resources: Local health clinics and charities may offer low-cost or free services.
1. Normal or High GFR (GFR ≥ 90)
- Description: In this stage, kidney function is still normal or only slightly reduced, but there is evidence of kidney damage, such as protein in the urine or structural abnormalities.
- Treatments & Medicines:
- Lifestyle Modifications: Focus on controlling risk factors such as high blood pressure, diabetes, and cholesterol.
- Dietary Changes: A balanced diet low in sodium, protein, and phosphorous may be recommended to reduce kidney strain.
- Regular Monitoring: Regular kidney function testing and urine protein checks.
- Find more about these dietary and lifestyle changes in Healthy Eating for Chronic Kidney Disease.
- Severity: Mild; no noticeable symptoms. Early detection is important to prevent progression.
2. Mildly Reduced GFR (GFR 60-89)
- Description: Kidney function is mildly reduced, and there is still kidney damage. Individuals may experience minimal or no symptoms.
- Severity: Mild; kidneys are still functioning adequately, but monitoring is required for potential progression.
3. Moderately Reduced GFR (GFR 30-59)
- Description: Kidney function is moderately reduced. Symptoms such as fatigue, swelling, and changes in urination may begin to appear. There is an increased risk of complications, such as high blood pressure and bone disease.
- Severity: Moderate; noticeable symptoms may start to appear, and the risk of progression to more severe stages increases.
4. Severely Reduced GFR (GFR 15-29)
- Description: Kidney function is severely reduced, and the kidneys can no longer maintain normal fluid, electrolyte, and waste balance. Symptoms may include difficulty concentrating, swelling, shortness of breath, and persistent fatigue.
- Severity: Severe; individuals are at high risk for end-stage kidney failure. Dialysis or a kidney transplant may be needed in the near future.
5. Kidney Failure (GFR < 15)
- Description: Kidney function is very low, and kidney failure has occurred. Waste products and fluids build up in the body, leading to severe complications. Dialysis or a kidney transplant is necessary to sustain life.
- Severity: End-stage renal disease (ESRD); life-threatening, requiring immediate intervention such as dialysis or a kidney transplant.
Where You Can Find More
For more information and support, visit these trusted resources:
- National Kidney Foundation
- American Kidney Fund
- Centers for Disease Control and Prevention – CKD
- Mayo Clinic – Chronic Kidney Disease
- World Kidney Day
More Resources on Chronic Medical Conditions:
Explore more resources on managing chronic medical conditions. Discover precision approaches for hypertension and heart health, advanced therapies for arthritis, diabetes, and cancer, and cutting-edge strategies for chronic kidney disease(CKD), COPD (Respiratory Problems). Learn about innovations addressing depression and cognitive issues like dementia and Alzheimer’s disease, and other cognitive challenges.
Share your experiences and learn from others in the community >> Join The Conversation: Chronic Kidney Disease For Older Adults.